Inside Binge Eating Disorder
What Science Is Revealing About a Common Condition
What Is Binge Eating Disorder?
Everyone overeats sometimes; at a celebration, during stress, or when food just tastes too good. But for people living with Binge Eating Disorder (BED), episodes of overeating feel different. They happen often, are difficult to control, and are usually followed by feelings of guilt, shame, or distress.
BED is a recognized medical condition, not a matter of willpower. It involves recurring episodes of eating unusually large amounts of food within a short period, often when not physically hungry. Unlike bulimia, these episodes are not followed by purging behaviors.
It’s one of the most common eating disorders in the United States, affecting both men and women across all ages and backgrounds.
What’s Happening Inside the Brain
Researchers believe BED involves complex interactions between brain chemistry, emotions, and behavior.
• Reward pathways: Eating triggers the release of dopamine, the brain’s “feel-good” chemical. For some individuals, this system becomes overstimulated or dysregulated.
• Stress and emotion: Anxiety, sadness, or trauma can intensify cravings or loss of control around food.
• Genetics and environment: Family history, dieting history, and cultural pressures about body image can all play a role.
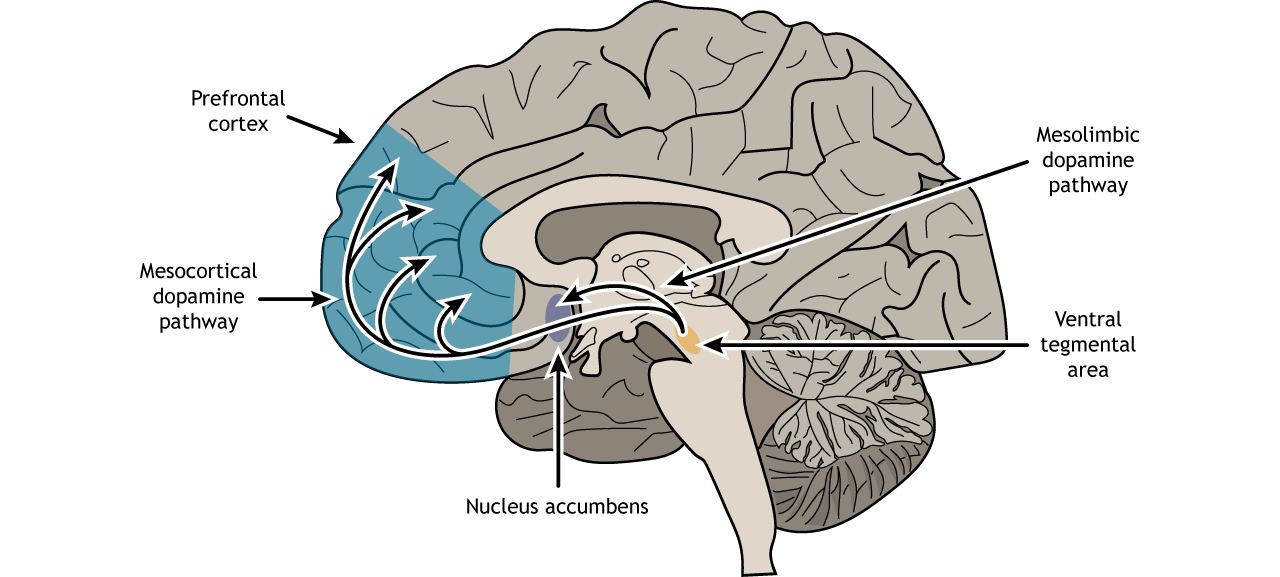
This combination of biology and environment helps explain why BED isn’t simply about self-control. It’s a condition that affects both the mind and body, and understanding it requires compassion and science working together.
Common Risk Factors
While anyone can experience binge eating behaviors, certain factors make the disorder more likely:
• Emotional distress or trauma
• Frequent dieting or restrictive eating patterns
• Low self-esteem or body dissatisfaction
• Family history of eating disorders or mental health conditions
• Biological factors affecting hunger hormones and reward systems

Recognizing these risk factors early can help people seek help before the cycle of overeating and guilt becomes more severe.
Current Ways to Manage Symptoms
Treatment for BED often combines several approaches:
• Cognitive behavioral therapy (CBT): Helps individuals identify emotional triggers and replace unhelpful thought patterns.
• Nutritional counseling: Promotes balanced, structured eating habits.
• Medication and medical supervision: Some patients benefit from medications that help regulate appetite or mood, always under the guidance of a healthcare professional.
• Support groups and community programs: Offer shared understanding and accountability.
• Mindfulness and stress management: Reduce emotional eating triggers and improve body awareness.
Because BED often overlaps with other conditions such as anxiety or depression, coordinated care is essential.

The Role of Clinical Research
Progress in understanding and treating Binge Eating Disorder depends on clinical research and on the individuals who choose to take part.
Clinical studies allow scientists to explore new treatment options, examine how the brain responds to hunger and emotion, and test therapies under carefully controlled, ethical conditions.
Each study is conducted under FDA and Institutional Review Board (IRB) oversight to ensure participant safety and confidentiality. While participating in a study does not guarantee personal benefit, each volunteer contributes to a growing body of knowledge that may help shape future care.
Living With BED: Practical Tips 💡
Managing Binge Eating Disorder takes time, support, and patience. Small, consistent actions can help individuals feel more in control and supported along the way:
• Keep regular meals and snacks to reduce extreme hunger.
• Identify emotional triggers and replace them with calming activities such as journaling, a walk, or deep breathing.
• Seek connection: Talking with a trusted friend or support group reduces isolation and shame.
• Focus on nourishment, not punishment: Shift attention from restriction to overall well-being.
• Celebrate progress: Even small changes in eating habits or self-talk deserve recognition.
Learn More About Local Research
To learn more or find out if you may qualify, contact the research team nearest you. Austin: ATXclinic@fstrials.com or 512-380-9595. Dallas: 214-361-7700